Written by Nia Imani-Pontes, CMSW, Service Coordinator, Mecklenburg County CDSA
Imagine you’re visiting with a family, and you and the parent observe the infant trying to pick up one of his toys. The mother shares that her son has been fussy for some time. Upon closer observation, you both notice that his hands are swollen, and each time you try to touch his hands, he screams. Maybe you’re working with a child that has begun to take steps, and he falls and starts crying. You notice his feet are swollen and painful to the touch. This mother shares that her child’s hematologist has provided her with information as to what to expect if her son develops the symptoms that are associated with dactylitis, or hand-foot syndrome. These are symptoms of a condition called sickle cell disease. Young children under the age of three with this diagnosis often have pain and swelling of their hands and feet that can last from two to ten days, sometimes with a fever. Treatment often consists of increasing intake of fluids and giving Tylenol for pain. Doctors may also recommend warm compresses or a heating pad to the area, but these can be difficult to use with a toddler. While most pain episodes can be handled at home, occasionally hospitalization is necessary. Imagine the impact on a child’s development with the frequency and duration of debilitating pain that is often a life- long pattern.
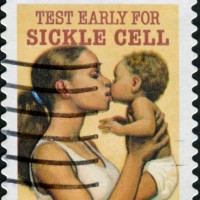
Who is affected by sickle cell disease? Here’s an overview to give you a bit more information.
Sickle cell disease is a group of hereditary red blood cell disorders characterized by oxygen deprivation on the cellular level. According to the Center for Disease Control and Prevention, the disease affects millions of people of all races worldwide, 90,000 – 100,000 Americans (1 in 500 African Americans). Once the roll of the genetic dice is complete, the results will determine what type of sickle cell disease a person has inherited. All complications of sickle cell disease can be traced to a mutation in a red blood cell gene that changes smooth, round blood cells into sickle-shaped cells that are stiff, sticky, and that tend to clump in the blood vessels. When they get stuck in small blood vessels, similar to a log jam, the sickled cells block blood flow to the limbs and organs, causing severe acute or chronic pain, serious infections, and organ damage over time, especially in the lungs, kidneys, spleen, and brain. The part of the blood cell called hemoglobin, which gives blood its red color because it contains iron, is responsible for carrying oxygen to all body parts. This is significant because another symptom of sickle cell disease is anemia. The average blood cell lives for approximately 120 days. Sickled cells are fragile, living less than 20 days. The resulting anemia often then causes fatigue. Because of the loss of oxygen to organs, and the subsequent damage caused over time, people with sickle cell disease potentially have shorter-than-average life expectancy.
As Early Interventionists, there are some things we can do to support children and families to help address their priorities and concerns:
- The team can help coordinate medical information and empower families to advocate for their children. Some issues that can come up include infection, episodic pain, jaundice, and delays in growth or development, to name a few.
- As you’re writing IFSP outcomes, be thinking about how some of the symptoms of sickle cell disease might come into play, such as temperature regulation, fatigue, or just general malaise. You can help the family better understand what to expect and plan their daily routines around these needs.
- We can also work with the family to help them cope with the daily unpredictability of the disease and crisis episodes.
- Families may have a lot of questions, and it’s important to be honest, especially if you don’t know the answer. Feel confident in saying that you would like to help them find the answers to their questions, and direct them to the appropriate medical supports when necessary.
The benefits of early intervention can be far-reaching for children with sickle cell disease. With the help of early intervention teams, medical and community support, children can enjoy better health and live a productive life.
Looking for more information? Here are some links to additional resources, and you can research camps in your area that are specifically for children diagnosed with sickle cell disease.
Cincinnati Comprehensive Sickle Cell Center – Donald Rucknagel, MD, PHD/Children’s Hospital Research Foundation
Your Child and Sickle Cell Disease – Sara Day, RN, MSN St Judes Children’s Research Hospital Hematology, Patient Education, and Biomedical Communications





No comments yet.